Diagnosing Low Testosterone: A comprenhesive guide

Testosterone is the principal male sex hormone, playing a vital role in the development of secondary sexual characteristics, libido, muscle mass, bone density, energy levels, and general well-being. Testosterone deficiency, also known as hypogonadism, can significantly impact a man’s physical and psychological health. Accurate diagnosis of hypogonadism is essential for determining appropriate treatment strategies. This guide provides a comprehensive overview of the diagnostic process for testosterone deficiency.
The Diagnostic Process
The diagnostic process of discovering low testosterone in males, usually consists of the following evaluations and assessments:
- Clinical Evaluation: A thorough medical history and physical examination are the first steps in diagnosing hypogonadism. Pertinent details for evaluation include:
- Symptoms: Low libido, erectile dysfunction, reduced energy levels, mood changes, decreased muscle mass, loss of body hair, gynecomastia (breast enlargement).
- Medications: Use of certain medications (e.g., opioids, corticosteroids) can suppress testosterone production.
- Underlying Conditions: Chronic illnesses like obesity, diabetes, sleep apnea, and pituitary disorders can contribute to low testosterone.
- Laboratory Assessment:
- Hormone Testing: Measurement of serum testosterone is the cornerstone of diagnosis. Guidelines recommend assessing the following:
- Total testosterone
- Free or bioavailable testosterone
- LH and FSH levels (to differentiate primary and secondary hypogonadism)
- Prolactin (if indicated)
- Testing Protocols: To ensure accurate results, testosterone is measured in a fasting state in the morning when levels are highest. It’s recommended to confirm low testosterone with repeat measurements on separate days.
- Hormone Testing: Measurement of serum testosterone is the cornerstone of diagnosis. Guidelines recommend assessing the following:
- Additional Investigations: In certain cases, further testing may be necessary to identify the underlying etiology of hypogonadism:
- Imaging: MRI of the pituitary region to assess for structural abnormalities.
- Semen Analysis: For evaluation of fertility status.
- Genetic Testing: In cases of suspected primary hypogonadism (testicular failure).
Interpretation of the results
The diagnosis of hypogonadism is based on the combination of consistent clinical symptoms and unequivocally low testosterone levels on repeated measurements. Healthcare providers will also consider the results of other hormone tests and imaging studies when determining the underlying cause. Differentiating between primary hypogonadism (originating from testicular dysfunction) and secondary hypogonadism (due to pituitary or hypothalamic dysfunction) is crucial for guiding management strategies.
Conclusion
A multifaceted approach is necessary for the accurate diagnosis of testosterone deficiency. Collaboration between patients and healthcare providers is essential to ensure appropriate evaluation, interpretation of findings, and individualized treatment plans.
Once and if diagnosed with low testosterone, you can consider exploring the available Treatment Options
Bonus content
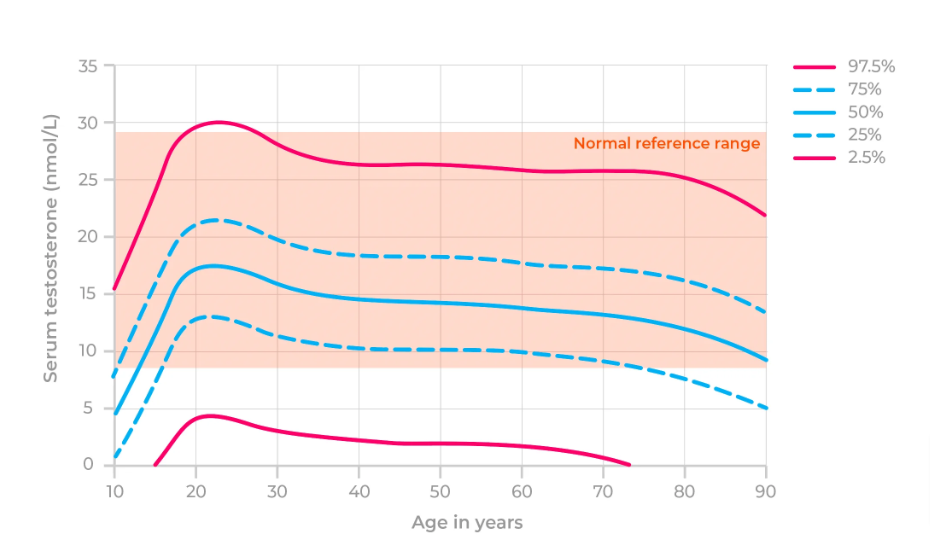
Normal Testosterone by age