Introduction to Testosterone

What is Testosterone?
Testosterone is often simplified as “the male sex hormone.” Technically accurate, this label overlooks its crucial role in many other bodily functions. A type of androgen, testosterone is primarily produced in the testicles with a small contribution from the adrenal glands. Women’s bodies also make testosterone but in significantly less quantity. This hormonal surge during puberty is the catalyst for major physical and sexual development in males.
Beyond sex, testosterone plays a significant role in:
- Bone health: Testosterone helps to build and maintain strong bones. As men age and testosterone levels decline, they are more at risk for osteoporosis.
- Muscle mass: Testosterone promotes muscle growth and strength. A decrease in testosterone can lead to a loss of muscle mass and strength.
- Red blood cell production: Testosterone stimulates the production of red blood cells, which carry oxygen throughout the body.
- Mood regulation: Testosterone may play a role in mood regulation. Low testosterone levels have been linked to symptoms of depression.
In men, testosterone levels naturally decline with age, potentially contributing to:
- Decreased muscle mass
- Decreased bone density
- Lower sex drive
Testosterone therapy is a treatment option for men with low testosterone levels. However, it’s important to note that testosterone therapy can have side effects and is not right for everyone. It’s important to talk to a doctor about the risks and benefits of testosterone therapy.
The impact of Testosterone
Testosterone’s influence extends far beyond sexual characteristics. Let’s look at its multifaceted effects:
- Physical Functions: Testosterone is a natural builder. It stimulates bone growth and maintains bone density, protecting men against fractures. Additionally, it functions as an anabolic agent, encouraging muscle development and strength. Healthy testosterone levels also influence fat distribution patterns and are vital for the production of red blood cells – the essential oxygen carriers of the body.
- Sexual Functions: Testosterone is the fuel for the male sex drive (libido), and is essential for achieving and maintaining erections. Furthermore, it is fundamentally involved in the production of healthy sperm.
- Cognitive Functions: Testosterone’s effects extend even to the brain. It influences mood, and low testosterone can lead to irritability, depression, or a general lack of well-being. There is some evidence it positively impacts focus and memory function as well.
Important Note: It’s vital to understand that both abnormally low and high testosterone levels can have negative health impacts. Maintaining healthy levels is crucial.
Production and Regulation of Testosterone
The production pathway
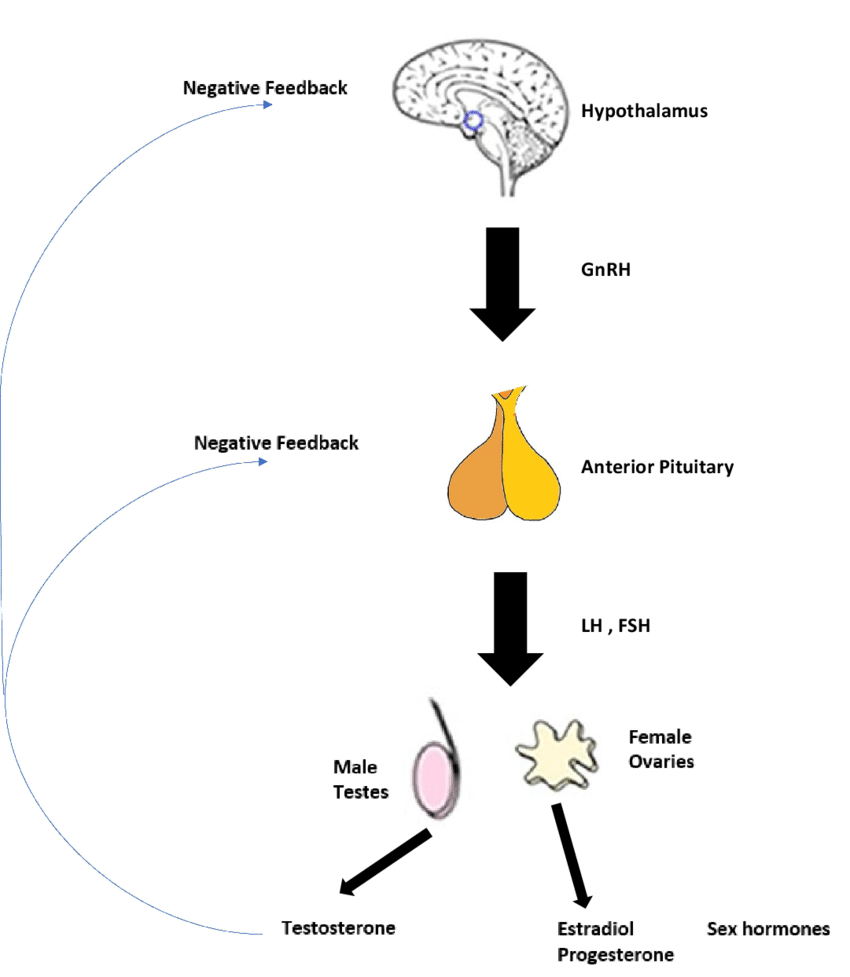
The body’s testosterone production system operates on an intricate feedback loop called the hypothalamus-pituitary-testicular (HPT) axis. Let’s break it down step by step:
- The Brain’s Command Center: The hypothalamus, a small but highly influential region of the brain, monitors testosterone levels in the bloodstream. When levels dip too low, the hypothalamus releases gonadotropin-releasing hormone (GnRH) in rhythmic pulses.
- The Pituitary Response: GnRH travels directly to the pituitary gland, a pea-sized gland at the base of the brain. Here, it stimulates the release of two essential hormones:
- Luteinizing Hormone (LH): LH journeys through the bloodstream to the testes, where it binds to receptors on Leydig cells. These specialized cells respond by synthesizing and releasing testosterone.
- Follicle-Stimulating Hormone (FSH): FSH targets cells within the testes called Sertoli cells, primarily stimulating sperm production. However, it also indirectly influences testosterone levels.
- The Feedback Loop: As circulating testosterone levels rise, they provide negative feedback to both the hypothalamus and pituitary gland. This signals them to decrease the production of GnRH, LH, and FSH, maintaining a balanced hormonal environment.
Factors affecting the natural Testosterone production
Testosterone isn’t produced in a vacuum. Numerous factors can influence its delicate balance:
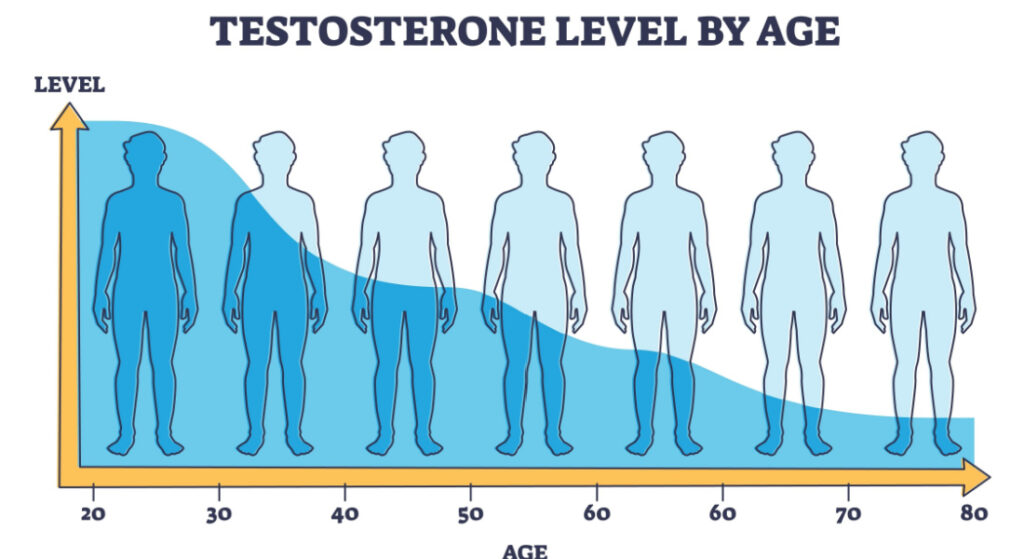
- Age: Testosterone levels naturally rise during puberty, peak in early adulthood, and then begin a gradual decline throughout a man’s life. Typically, around age 30, there’s a subtle but steady decrease of approximately 1% per year.
- Lifestyle Factors:
- Diet: Consuming a balanced diet rich in zinc, healthy fats, and vitamin D can support optimal testosterone production.
- Exercise: Regular physical activity, particularly strength training, has been associated with increased testosterone. Conversely, both extreme overtraining and a sedentary lifestyle can negatively impact production.
- Sleep: Lack of sufficient, quality sleep disrupts the body’s hormonal balance, including testosterone production.
- Stress: Chronic stress elevates cortisol levels, which can suppress testosterone production. Implementing stress-management techniques is beneficial for overall hormonal health.
- Medical Conditions:
- Obesity: Excess adipose tissue converts testosterone into estrogen, leading to a hormonal imbalance.
- Testicular Issues: Conditions like injury, undescended testicles, or infections can directly disrupt the testes’ ability to produce testosterone.
- Pituitary Disorders: Disorders affecting the pituitary gland can impair the release of LH and FSH, indirectly affecting testosterone production.
- Other Medical Conditions: Chronic illnesses like kidney failure, liver disease, type 2 diabetes, or sleep apnea can influence testosterone levels.
- Medications: Certain medications, like corticosteroids or anabolic steroids, can disrupt the natural testosterone production process.
Testosterone Levels
Testosterone is a hormone produced primarily in the testicles in men and, to a lesser extent, in the ovaries in women. It plays a crucial role in male sexual development, fertility, muscle mass, bone density, and overall well-being. Understanding testosterone levels is essential for maintaining optimal health and addressing potential imbalances.
Measuring Testosterone
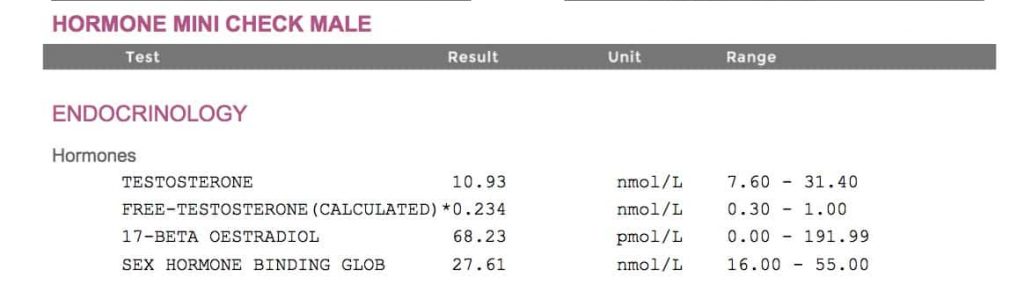
There are several types of tests available to measure testosterone levels, each providing specific information:
- Total Testosterone: This test measures the combined amount of testosterone that is bound to proteins and free (unbound) in the bloodstream.
- Free Testosterone: This test measures the amount of testosterone that is not bound to proteins and is readily available for tissues to use.
- Bioavailable Testosterone: This test measures the combination of free testosterone and testosterone that is loosely bound to albumin, which can dissociate and become bioavailable.
Understanding Reference Ranges
When interpreting testosterone levels, it is essential to consider the reference ranges provided by the laboratory. These ranges can vary based on factors such as age, gender, and the specific testing method used. Generally, the following ranges are considered normal for adult males:
- Total Testosterone: 300 to 1000 ng/dL (10.4 to 34.7 nmol/L)
- Free Testosterone: 5 to 21 pg/mL (0.17 to 0.73 nmol/L)
- Bioavailable Testosterone: 110 to 575 ng/dL (3.8 to 20 nmol/L)
It’s important to note that these ranges are broad guidelines, and individual variations may occur. Consulting with a healthcare professional is recommended for a comprehensive evaluation and personalized interpretation of test results.
What is Low Testosterone (Hypogonadism)?

Low testosterone, also known as hypogonadism, is a condition characterized by insufficient testosterone production. There are two main types of hypogonadism:
- Primary Hypogonadism: This type occurs when the testicles themselves are unable to produce sufficient testosterone. It can result from conditions such as Klinefelter syndrome, injury, radiation therapy, or certain genetic disorders.
- Secondary Hypogonadism: In this case, the problem lies in the hypothalamus or pituitary gland, which regulates testosterone production. Causes may include pituitary tumors, obesity, chronic illnesses, or excessive stress.
Causes of Low Testosterone
Several factors can contribute to low testosterone levels, including:
- Aging: Testosterone levels naturally decline with age, a condition known as “andropause” or male menopause.
- Obesity: Excess body fat can lead to increased conversion of testosterone to estrogen, lowering testosterone levels.
- Chronic Illnesses: Conditions like type 2 diabetes, chronic kidney disease, and HIV/AIDS can disrupt testosterone production.
- Medications: Certain medications, such as chemotherapy drugs, opioids, and corticosteroids, can suppress testosterone levels.
- Injuries or Tumors: Damage to the testicles or pituitary gland can impair testosterone production.
Symptoms of Low Testosterone
Low testosterone levels can manifest in various physical, sexual, and mental/emotional symptoms:
Physical Symptoms:
- Decreased muscle mass and strength
- Increased body fat, particularly around the abdomen
- Decreased bone density, increasing the risk of osteoporosis
- Fatigue and low energy levels
- Hot flashes and night sweats
Sexual Symptoms:
- Reduced libido (sex drive)
- Erectile dysfunction
- Infertility or reduced sperm production
Mental/Emotional Symptoms:
- Mood changes, including irritability, depression, and lack of motivation
- Difficulty concentrating or memory problems
- Sleep disturbances
For further research and information, you can refer to reputable sources such as:
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/male-hypogonadism/symptoms-causes/syc-20354778
- Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/15660-low-testosterone-male-hypogonadism
- Harvard Health Publishing: https://www.health.harvard.edu/drugs-and-medications/testosterone-for-men-with-low-levels
These sources provide in-depth information, research findings, and expert insights on testosterone levels, hypogonadism, and related topics.
Diagnosing Low Testosterone
Identifying and properly diagnosing low testosterone levels is crucial for implementing effective treatment and managing potential associated health risks. While symptoms may suggest a hormonal imbalance, it is essential to seek professional medical guidance and avoid self-diagnosis.
Importance of Professional Diagnosis
Self-diagnosis of low testosterone can be problematic as many symptoms, such as fatigue, decreased libido, and mood changes, are non-specific and can be attributed to various underlying conditions. Only a qualified healthcare professional can accurately evaluate your situation and determine the appropriate course of action.
The diagnostic process typically involves a thorough medical history, physical examination, and laboratory tests. Your healthcare provider will inquire about your symptoms, medical conditions, medications, and lifestyle factors that may contribute to hormonal imbalances. A comprehensive physical examination can help identify potential causes or related issues.
Blood tests are a crucial component of the diagnostic process. Typically, a healthcare provider will order a total testosterone test, which measures the combined amount of testosterone bound to proteins and free in the bloodstream. However, due to variations in testosterone levels throughout the day, repeat testing may be necessary to confirm the initial findings.
Interpreting results
When evaluating testosterone levels, it is essential to consider the results in the context of your symptoms, age, and overall health status. Low testosterone levels alone do not necessarily indicate a need for treatment, as some men may experience few or no symptoms despite having slightly low levels.
Conversely, some men may exhibit symptoms of low testosterone despite having levels within the normal range. In such cases, additional testing may be required to assess the bioavailable or free testosterone levels, which represent the amount of testosterone readily available for use by the body’s tissues.
Additional Testing
In some instances, further testing may be necessary to determine the underlying cause of low testosterone and develop an appropriate treatment plan. These additional tests may include:
- Imaging Studies: Techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can help identify structural abnormalities or tumors in the pituitary gland or testicles that may be contributing to hormonal imbalances.
- Additional Hormone Panels: Evaluating other hormones, such as luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin, can provide insights into the root cause of low testosterone and assist in distinguishing between primary and secondary hypogonadism.
- Genetic Testing: In certain cases, genetic testing may be recommended to identify potential inherited conditions or chromosomal abnormalities that could be impacting testosterone production.
Feel free to continue reading our detailed guide about low Testosterone diagnosis on our Diagnostic Journey section
Testosterone Replacement Therapy (TRT) Basics
What is TRT?
Testosterone Replacement Therapy (TRT) is a medical treatment designed to restore testosterone levels in men suffering from hypogonadism – a condition where the body fails to produce sufficient amounts of testosterone. TRT delivers bioidentical testosterone (chemically the same as naturally produced testosterone) to the body, supplementing what it can no longer make adequately on its own.
Who is TRT for?
TRT is not a solution for everyone. It’s specifically intended for men diagnosed with clinically low testosterone accompanied by symptoms that affect their quality of life. These symptoms might include:
- Reduced libido (sex drive)
- Erectile dysfunction
- Decreased energy levels and fatigue
- Muscle loss and increased body fat
- Mood changes, irritability, and potential depression
- Decreased cognitive function (focus, memory)
Forms of TRT
Several methods exist to deliver testosterone:
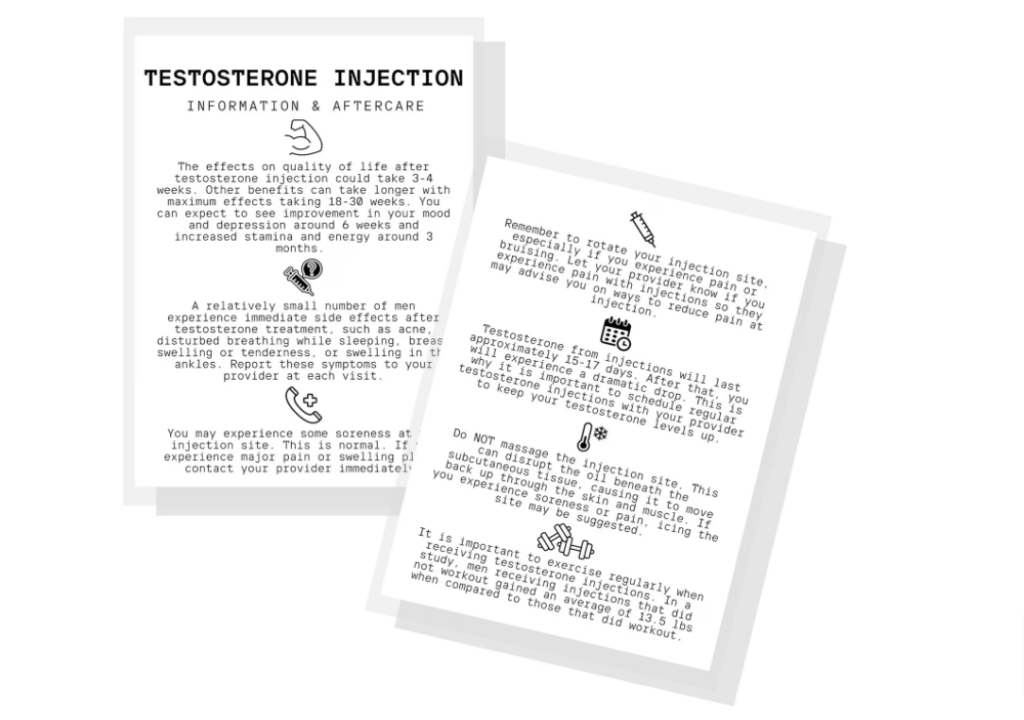
- Injections: The most common TRT method, injections of testosterone are administered into a muscle, typically once every one to two weeks. Injections offer reliable absorption and predictable testosterone levels.
- Gels/Creams: Topical testosterone gels or creams are applied daily to areas like the shoulders, upper arms, or abdomen. They provide a more gradual release of testosterone but require diligence to prevent accidental transfer to others.
- Patches: Patches containing testosterone are worn on the skin, replaced daily. Similar to gels and creams, they provide a steady-release of testosterone.
- Implants: Small testosterone pellets are surgically implanted under the skin, releasing a consistent dose of testosterone over several months. Implantation is a minor procedure but necessitates replacement every few months.
Pros and Cons of Each Method
Each form of TRT has advantages and disadvantages your doctor will help you consider. Factors like cost, convenience, side effect profiles, and personal preferences will all play a role in the decision.
Starting TRT
What to expect at initial appointments:
If you suspect low testosterone, consult a doctor specializing in hormone therapy. Here’s what to expect:
- Comprehensive Discussion: You’ll discuss your symptoms, medical history, and lifestyle.
- Blood Work: Testosterone levels are checked through blood tests, typically on more than one occasion. Further blood work may be needed to rule out other medical conditions.
- Personalized Treatment Plan: If TRT is indicated, your doctor will discuss the different forms of therapy, potential benefits, risks, and side effects, and help tailor a plan for you.
Importance of Finding a Qualified Physician
TRT requires ongoing monitoring and dose adjustments under the care of an experienced medical professional. Look for a doctor who specializes in hormone replacement therapy or men’s health to ensure safe and effective treatment.
If you would like to find out more information, follow our Treatments & Options section.
Potential Benefits of TRT
While the benefits of TRT can vary from person to person, medically supervised therapy holds promise in several key areas
Improved Physical Health
- Muscle Mass and Strength: Testosterone is a natural anabolic agent that plays a crucial role in building and maintaining muscle mass. TRT can help men with low testosterone regain lost muscle and improve overall strength.
- Energy Levels: Chronic fatigue and lack of energy are common symptoms of low testosterone. TRT can potentially increase energy and reduce feelings of sluggishness.
- Bone Density Testosterone plays a vital role in keeping bones strong and healthy. TRT can help improve bone density, reducing the risk of osteoporosis and fractures in men with hypogonadism.
Enhanced Sexual Function
- Libido: Low testosterone frequently leads to a decline in sexual desire. TRT often boosts libido, restoring a healthy sex drive.
- Erectile Function: Testosterone is necessary for achieving and maintaining erections. TRT can significantly improve erectile function in men with low testosterone.
- Fertility: In cases where low testosterone is the underlying cause of infertility, TRT may improve sperm production and overall fertility potential.
Mental and Emotional Well-being
- Mood: TRT can have a positive impact on mood, reducing irritability, anxiety, and symptoms of depression in men with low testosterone.
- Focus: Some studies suggest TRT may improve cognitive function, including focus, concentration, and memory.
- Sleep: Restoring healthy testosterone levels can improve sleep quality, which is often disrupted in men with low testosterone.
- Self-esteem: The combined physical, sexual, and emotional improvements associated with TRT can lead to a boost in confidence and overall self-esteem.
Important Considerations
It’s crucial to remember that TRT is not a magic solution for all men. The benefits are most significant in those with clinically diagnosed hypogonadism. Individual responses may vary, and TRT carries potential risks.

